President’s Blog July 2016
Recently the college published a key report entitled ‘Why does winter in A&E get worse every year’. The report is on our website but appreciating that time is a scarce commodity I have summarized some of the key messages here. A similar summary was recently published in ‘The House’ magazine – a publication circulated to all MPs and Peers.
Attendances and Admissions
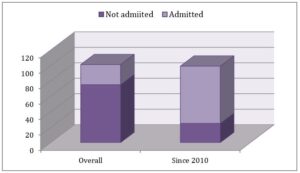 Patient attendances have risen steadily in the last five years creating an increase in workload equivalent to ten medium sized A&E departments. Previously about one in four A&E attendances led to an admission but remarkably of the 611,250 extra attendances since 2010, three out of four have required admission! It is therefore clear that planning to redirect such patients is unlikely to succeed.
Patient attendances have risen steadily in the last five years creating an increase in workload equivalent to ten medium sized A&E departments. Previously about one in four A&E attendances led to an admission but remarkably of the 611,250 extra attendances since 2010, three out of four have required admission! It is therefore clear that planning to redirect such patients is unlikely to succeed.
Demographics
Data from Public Health England show the number of people over 85 years will grow by 90,000 per year for the next 20 years. Compared to 2011 there are an additional 500,000 people aged over 85 alive today. Whilst we welcome this it must also be noted that the probability of admission to hospital is directly correlated with age; if a person over the age of 80 presents to A&E they have an 80% probability of being admitted.
With fewer acute beds in 2015 than 2010 these capacity pressures will continue to defeat current strategies. Whilst more can be done to reduce the number of frail elderly admitted and even more can be done to reduce their length of stay, recognizing that on average patients aged over 80 have at least six long term conditions at the time of admission highlights the complexity of this challenge.
Lack of alternatives
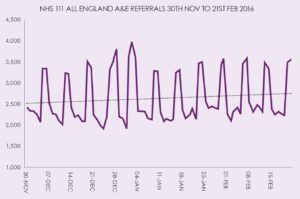 The availability of 7-day services is often referred to. The chart shows the number of patients referred to A&E by NHS 111 by day of week this winter. The peaks represent weekends and indicate that at weekends the NHS does not provide the most appropriate services – instead and in large measure A&E is the only available service
The availability of 7-day services is often referred to. The chart shows the number of patients referred to A&E by NHS 111 by day of week this winter. The peaks represent weekends and indicate that at weekends the NHS does not provide the most appropriate services – instead and in large measure A&E is the only available service
Pressures on staff
Recognition of the pressures on staff is seldom acted upon. The four hour standard is a barometer of patient care but it also indicates staff pressures. Plotting the four hour data as a proxy indicator of this pressure shows just how challenged working in our A&E departments has become.
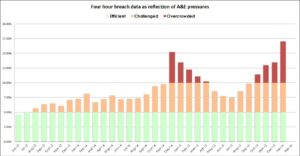
Since the winter of 2014 most of the time has been spent in the ‘red zone’ where breaches and pressures are double the accepted level.
These pressures take their toll on retention as staff seek to find more sustainable careers. We have already lost 450 registrars. Collectively this cohort would have been able to attend to almost 1 million patients per year! The loss of such a valuable resource is an indictment of workforce planning and support. We are left with the invidious spectacle of rising locum costs and unsafe services leading to A&E closures.
Winter all year
It is evident that current pressures on A&E have very little relationship to the seasons.
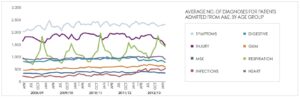
In fact the only thing that actually changes in winter is a doubling of patients admitted with respiratory illness; nevertheless in a system so limited in capacity and resource it takes very little to ‘tip over’.
As summer progresses I hope all of you have plans in place for a well earned break. My tenure as President draws to a close with the handover at our AGM, I hope to see many of you at Bournemouth for what promises to be another outstanding Annual Scientific Conference.



0 Comments