What’s behind the increase in demand in Emergency Departments?
This analysis is the first instalment of RCEM’s acute insight series. The series aims to use data and evidence to analyse and explain trends in Emergency Department activity. If you have any questions, please get in touch with policy@rcem.ac.uk
Levels of Emergency Department (ED) attendances and subsequent admissions are not only reaching pre-pandemic levels but surpassing them. In June 2021, attendances to Type 1 EDs were the highest on record whilst admissions were the second highest since the start of the pandemic. Alongside this increase in demand, covid-19 hospitalisations remain fairly low which raises the question – why are we experiencing winter pressures during the spring and summer months?
As lockdown restrictions have begun to ease, we have seen a rise in the number of covid-19 cases, yet these are largely not translating into hospitalisations. As of 21 July 2021, NHS Syndromic Surveillance Data shows that there are around 250 attendances to EDs per day across England that are recorded as ‘covid-19-like’, compared to 1000 covid-19-like attendances recorded at the end of January. Similarly, the number of admissions to hospital and diagnoses in hospital have drastically decreased in the same timeframe; as of 10 July, there were 442 covid admissions to hospital per day, compared to over 4000 in January. Clearly a spike in covid-19 infections cannot be solely to blame for the increase in demand over the past few months.
Lack of access to Primary Care
The pandemic has altered the way that the public accesses primary and community healthcare services. Since the first lockdown, most primary care services have become virtual, meaning that people are now accessing their GP through online bookings, video, and phone consultations.
56% of GP appointments in May 2021 were carried out face-to-face, compared to 80% in January 2020. There was a corresponding rise in phone appointments from 14% to 40% in the same time period.[1] [2] In many cases, this has made accessing healthcare quicker and easier for people, however this format of healthcare does not come without its setbacks. Many groups risk becoming excluded, including older people, disabled people, those from deprived areas or who are on low incomes, and those whose first language is not English. For example, the GP Patient Survey from July 2021 found that only 52% of respondents had a GP appointment within the last six months, compared to 70-72% in the preceding three years.
Furthermore, many people are still struggling to access primary care or finding that it does not fit their needs, as they are worried that their health issues are not being accurately diagnosed[3]. The Richmond Group of Charities conducted a qualitative study on attitudes towards health services throughout the pandemic and found that many participants described getting an appointment to be ‘impossible’ and instead found emergency or walk-in services to be a better option for them.[4] The 2021 GP Patient Survey further supports this finding; in the first half of 2021, 8% of patients that could not or did not take a GP appointment attended an ED instead and 26% of those who tried to book a GP appointment, but their practise was closed, subsequently attended an ED if they chose to contact another NHS service. The volume of people attending primary care each month means that small changes such as this can have significant impacts on the rest of the health service. Small deteriorations in the number of people accessing appropriate GP consultations have the potential to put great pressure on the urgent and emergency care system.
The RCGP have also voiced this sentiment; a poll conducted by the College in September 2020 found that 90% of GPs felt they could be efficient in delivering the best health outcomes all or most of the time through face-to-face consultations, compared to 75% over the phone and only 46% via video.[5] Maintaining the balance between virtual and in-person primary care services is integral in ensuring that people can access healthcare when and how they want and feel satisfied with the care that they receive. In turn, they will not feel the need to turn to the urgent and emergency care system when they would be better treated elsewhere.
Conversely, the ease of accessing GP services virtually for many groups has probably led to greater demand from patients and made access harder for other patients. By removing some of the barriers that previously existed in accessing primary care (for example, the average waiting time for a GP appointment before the pandemic was two weeks), an increasing number of people are contacting GP services, many of whom have only low acuity and self-limiting problems.
Furthermore, General Practice has significant workforce challenges. The RCGP have recently called for an emergency rescue plan as there are not enough GPs to keep up with demand from the fallout of the pandemic alongside a growing and ageing population; the number of full-time equivalent GPs has fallen by 4.5% since September 2015 yet GP consultation rates were 11% higher in June 2021 compared to June 2019. All parts of the healthcare service are interconnected and therefore “if general practise collapses, the rest of the NHS will follow not far behind it”.[6]
Phone-first services
A similar phenomenon is occurring in NHS 111 and other phone-first services. In April 2021, NHS 111 experienced the largest numbers of calls received and triaged, standing at 1,877,584 and 1,531,301 respectively. 189,664 callers were recommended to attend an ED meaning that 12.4% of calls that were triaged were streamed towards ED services. Prior to May 2020, this percentage almost always remained under 10% but has begun to rise throughout the pandemic and at an increased rate over the past few months. While a 2.5% increase may not seem significant, NHS 111 is a high-volume system, and this percentage increase can translate to almost 100,000 more recommendations, as seen between April 2020 and April 2021.
Moreover, this figure should be considered in conjunction with recommendations to ambulance services; in May 2021, 11.5% of triaged calls were recommended to the ambulance service, many of which would have then been directed to an ED. Therefore, as many as 24% of triaged NHS 111 callers could be attending EDs.
The purpose of NHS 111 is to give the public advice and make it easier for them to access healthcare services during times of urgency. Therefore, it would be expected that callers are directed to the most appropriate form of healthcare, limiting demand in EDs from patients who do not need to be there. However, the increase in people being recommended to EDs coincides with a decrease in the percentage of ED attendances which are being admitted. In June 2021, the percentage of attendances admitted stood at 27.9%, the lowest since July 2017 (27.1%). This implies that many patients who are presenting at EDs are low acuity, and the reasons why they are attending are due to inaccurate recommendations from 111 or primary care, or dissatisfaction with other services.
It is currently uncertain whether the NHS 111 First pilot, by which low acuity patients are encouraged to phone NHS 111 from an ED has been effective at reducing ED attendances. The evaluation has not been published at the time of writing.
Healthwatch carried out a poll in order to understand public attitudes towards 111 and people’s experiences with it. Experiences varied vastly, although they found that there were overall issues with the public’s confidence in the call handlers and service integration overall. One respondent claimed:
“I called 111 for advice …. I gave full details and thought they would be able to give guidance on the phone but they booked me an appointment at A&E. A&E were not interested & sent me home, saying nothing to worry about. They seemed surprised 111 had sent me.”[7]
Moreover, RCEM recently conducted a workforce survey of our members to find out more about how Emergency Medicine Clinicians have handled the pandemic and what they think could be done to improve the specialty. Regarding a question we asked on phone-first services and demand, an overwhelming 50.7% of people responded that it had increased or significantly increased demand in their ED, while only 3.6% responded that it had decreased or significantly decreased demand, showing that this service is currently not fulfilling its purpose.
For both virtual GP consultations and 111 services, the availability of these services may have led to supply induced demand, which refers to the increase in attendances or engagement with healthcare services which would have not occurred had the initial service not been available. Therefore, initiatives that aim to reduce or manage demand often have unintended consequences.
Mental illness
This patient group needs separate consideration as they suffer very long stays in emergency departments and often receive fragmented and sub-optimal care. The deterioration in people’s mental health throughout the course of the pandemic can be seen as a result of the multiple lockdowns, wherein people may have become more isolated and anxious, partnered with the difficulty in accessing mental health services. Between June 2019 and March 2020, 10% of adults were experiencing moderate to severe symptoms of depression but by June 2020, this had almost doubled to 19%.[8] Similarly, a survey released by Public Health Wales in May 2021 found that 42% of people felt that their mental health is worse now than before the pandemic, with women and young people more likely to have experienced a decline in their mental health.
The way that mental health services were carried out changed at the beginning of the pandemic; likewise to primary care, appointments moved from face-to-face to video and telephone calls which are not always appropriate and can act as a barrier to services, particularly for the more seriously ill patients. The increase in the number of people experiencing mental health issues meant that many people were unable to access support until their condition had worsened due to the high levels of demand. As the graph below highlights, there has been a significant decrease in the number of people accessing mental health services since the start of the pandemic.
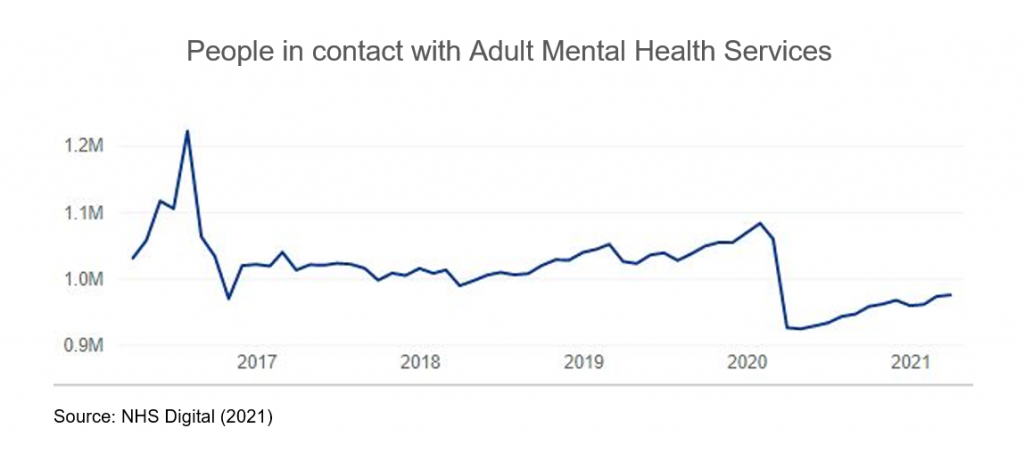
This limited community support alongside fewer inpatient beds have meant that there has been significant unmet need throughout the pandemic, which is subsequently leading to great numbers of people accessing services only once they are in crisis. The CQC have found that some EDs have been functioning as a ‘first contact’ for people in mental health crisis due to a lack of alternatives.[9] Therefore, not only are there more people facing mental health issues, but people are experiencing more serious and acute issues due to the lack of timely treatment available. This has led to a greater reliance on ED services and a greater number of mental health presentations to EDs.
Elective backlog
Demand in EDs and the elective backlog are closely related. During the first wave of the pandemic, all planned elective surgery was cancelled, leading to a substantial backlog of patients, the recovery of which has only just begun. As of May 2021, there were 5.3 million people on the elective surgery waiting list, the highest figure on record, with over 336,000 people waiting for more than a year.
Alongside fewer patients being treated, six million fewer people were referred into consultant-led elective care in 2020 compared to 2019.[10] These people have been described as ‘missing patients’ and remain an unknown in the recovery of the elective backlog. It is highly likely that many people are now beginning to attend EDs and access other healthcare services again as fear of covid has largely diminished or because their conditions have significantly worsened due to the lack of clinical oversight. People are not only presenting to EDs due to complications relating to their delayed procedures but those who delayed accessing healthcare last year as a result of the pandemic are now attending EDs again with potentially more serious issues.
Young people
One group that has disproportionately increased demand in EDs over recent months is children and young people. This is partly because there are high numbers of young children acquiring infections that are usually seen in the winter months, as a result of the easing lockdown restrictions. Many parents are taking their young children with mild fevers to EDs rather than seeking help at GPs, pharmacies, or NHS 111 because they are worried about these symptoms that they have potentially not experienced in their child before. One consultant paediatrician has said, “We’re seeing three times the number of children with fevers for early June than in 2020… and twice the number of children we saw in June 2019, significantly higher than we’ve ever seen before.” This fear over their child’s health partnered with potential difficulty in accessing other services or being streamed towards the urgent and emergency care system has consequently led to a drastic increase of young people attending EDs.
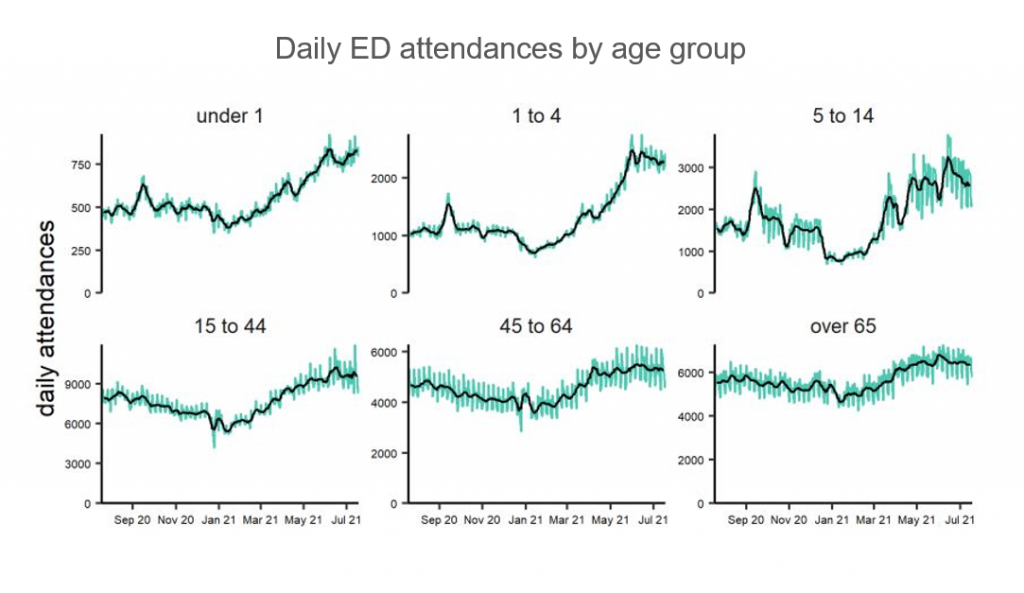
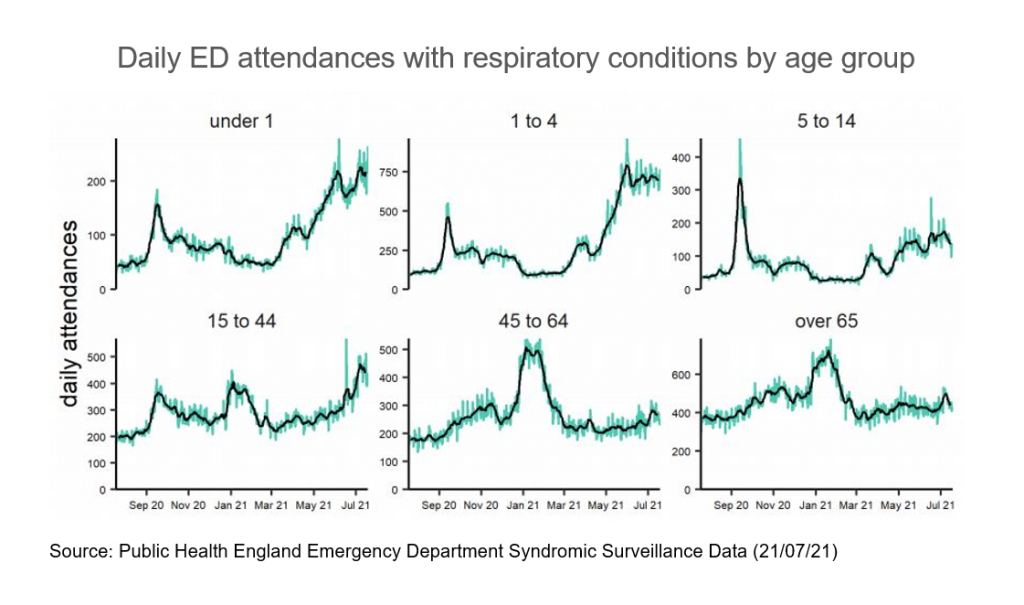
In addition, there is a real threat that flu and RSV outbreaks will drive further demand. Circulation of flu and RSV were very low during winter 2020/21 due to lockdown restrictions and social distancing, so there is an increasing chance that these respiratory infections could re-emerge more strongly as we move into the winter months due to diminishing population immunity.[11] This is likely to affect young children more intensely as they have not been exposed to these infections before. Therefore, it is expected that this demand in EDs will continue to increase.
Looking forward
Whilst the increase in demand is not directly related to covid cases, the indirect effect of the pandemic has led to more people turning to EDs for healthcare. Emergency Departments are not only experiencing winter pressures in the summer months, but they are surpassing attendance records, causing crowding and poor care. While NHS staff have continually showed their resilience throughout the pandemic, this way of working is not sustainable and can lead to increased rates of burnout in the Emergency Medicine workforce. Our recent workforce survey on our membership found that 50% are considering reducing their working hours in the next two years, largely due to workforce pressures and burnout. If action is not taken to manage demand and improve capacity in EDs, winter will be extremely challenging.
While this blog explains increased demand, this is only half of the story. Hospitals are still facing a decreased bed stock and Infection Prevention Control measures are still in place. This means that EDs have a diminished ability to handle increases in demand, and when demand does rise, patients are more likely to experience care in unsafe conditions. The next worrying phase of the pandemic will be the expected resurgence of flu and RSV this winter alongside rising covid-19 cases. This will create further significant challenges for EDs during a time of year when demand increases anyway. Not only does there need to be an expansion within hospitals and EDs to keep up with these levels of demand, but all parts of the healthcare system – including primary care, mental health, and community care – require additional capacity so patients can access the right kind of care at the right time.
Kelly Sarsfield, Policy Administrator
Adrian Boyle, Vice President Policy
[1] NHS Digital (2021). https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice/may-2021
[2] NHS Digital (2021). https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice/may-2021
[3] Healthwatch (2021). https://www.healthwatch.co.uk/news/2021-03-22/gp-access-review-must-be-part-nhs-covid-19-recovery
[4] Richmond Group of Charities (2021). https://richmondgroupofcharities.org.uk/sites/default/files/richmond_group_phase_3_report_final_july_2021.pdf
[5] Royal College of General Practitioners (2021). https://www.rcgp.org.uk/about-us/news/2021/may/gp-consultations-post-covid.aspx
[6] Royal College of General Practitioners (2021). College sounds SOS for general practice – and calls for rescue plan (rcgp.org.uk)
[7] Healthwatch (2021). https://www.healthwatch.co.uk/blog/2021-03-09/nhs-111-first-making-difference
[8] Nuffield Trust (2020). https://www.nuffieldtrust.org.uk/news-item/what-impact-has-covid-19-had-on-mental-health-services
[9] Care Quality Commission (2020). https://www.cqc.org.uk/news/releases/cqc-finds-mental-health-inpatient-services-coped-well-coronavirus-covid-19-there-will
[10] The Health Foundation (2021). https://www.health.org.uk/news-and-comment/charts-and-infographics/how-is-elective-care-coping-with-the-continuing-impact-of-covid-19
[11] Academy of Medical Sciences (2021). Winter viruses and COVID-19 could push NHS to breaking point, warns new report | The Academy of Medical Sciences (acmedsci.ac.uk)



0 Comments